Abstract
Background and aims:
Angioimmunoblastic T-cell lymphoma (AITL) is currently classified amongst an umbrella group of diagnoses referred to as nodal peripheral T-cell lymphoma (PTCL) with T-follicular helper (TFH) phenotype. In this entity, it is recognized that the presence of atypical B-cell blasts mimicking Hodgkin-Reed-Sternberg cells may lead to misdiagnosis as Hodgkin lymphoma (HL), resulting in suboptimal management and poorer outcomes. This diagnostic complexity has been acknowledged by the World Health Organization classification of lymphoid neoplasms. In this study, we aim to investigate the clinical features and outcomes of such cases of diagnostic ambiguity (HL/PTCL).
Methods:
A total of 379 patients from the Singapore Lymphoma Study database across three tertiary cancer centers (National Cancer Centre Singapore, Singapore General Hospital, National University Cancer Institute) were included in this study, including those diagnosed with AITL (n=169), HL (n=178) and HL/PTCL (n=32). Median follow-up was 47.5 months. Relevant demographical and clinical characteristics were collected. Survival analyses were performed using the Kaplan-Meier method.
Results:
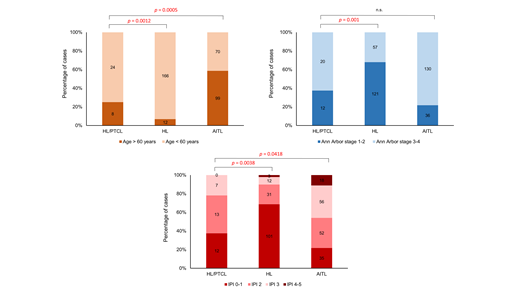
The 32 patients with HL/PTCL were identified from three distinct clinical scenarios. In the first group (n=18), an initial histological diagnosis of HL was revised upon independent pathological re-assessment following a second opinion consultation (revised diagnoses to AITL, n=10; PTCL-TFH, n=7; PTCL-NOS, n=1). In the second group (n=11), the histological diagnoses were different at diagnosis and at relapse (mostly HL relapsed as AITL/PTCL-TFH, n=9). The third group consisted of patients with synchronous or composite features of both HL and AITL/PTCL at diagnosis (n=3). In the overall cohort, most were male (62.5%), and the majority had excellent performance status with ECOG 0-1 (96.9%). The median age was 45 years (range, 20 to 77), which is older than the HL cohort (28 years, p=0.0012) but younger than the AITL cohort (62 years, p=0.0005). In terms of disease staging, most were Ann Arbor stage 3-4 (62.5%), which is comparable to the AITL cohort (78.3%), but significantly more advanced than the HL cohort (32%, p=0.001). HL/PTCL represented a group with worse prognostic risk scores by IPI as compared to HL (p=0.0038), but better as compared to AITL (p=0.0418). Accordingly, the median overall survival was 8.4 years for HL/PTCL, compared to 5.5 years (AITL) and not reached (HL) (logrank p<0.0001).
Conclusion:
We describe a significant and clinically distinct group of HL and AITL/PTCL-TFH cases which are challenging to diagnose. Further studies on the molecular characteristics of this ambiguous disease entity may be required to resolve the diagnostic difficulties.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal